Download the presentation on the topic of herpes virus. Department of Medical Biology, Microbiology, Virology and Immunology Adenoviruses. Herpesviruses Assoc. Tkachuk N.I. “Bad news in a protein shell” by P. Medawar
Slide 1

Slide 2
The herpes virus is a silent companion of our body
Herpes is a small blistered rash, most often on the lips or nose, popularly called a “fever” or “cold.” The name "herpes" comes from the ancient Greek word "herpain" ("to crawl"). This is a characteristic property of herpes: from a single small vesicle to spread throughout the body.

Slide 3
“Bad news in a protein shell” by P. Medawar
Herpes viruses can be asymptomatic in people with a normal immune system, but in people with immunosuppression they can cause severe illness and death. Once the herpes virus enters the body, it remains there forever.

Slide 4
According to WHO:
Herpes is one of the most common human viral infections. 95% of people globe infected with herpes simplex virus (HSV), up to 20% of them have some active clinical manifestations of the infection. Mortality from herpetic infections among viral diseases is in second place (15.8%) after hepatitis (35.8%); The frequency of herpes on the lips varies from person to person and can recur from 2 to 12 times a year.

Slide 5
Epidemiology of the herpes virus
Epidemiological studies show that herpes is widespread. Humoral immune response is accompanied mainly by the production of antibodies to antigens. Serological reactions in which the virus itself is used as an antigen - complement fixation, neutralization, indirect hemagglutination, indirect immunofluorescence, RIA and ELISA - do not allow us to determine what type of herpes virus is causing the infection. Herpes simplex virus type 1 is infected earlier and more often than herpes simplex virus type 2. More than 90% of people over 40 years old have antibodies to herpes simplex virus type 1.

Slide 6
The structure of the herpes virus
DNA virus; The icosahedron-shaped viral capsid consists of 162 capsomeres; The diameter of the outer shell of the virus is 180 nm, the diameter of the viral nucleocapsid is 100 nm. The outer envelope of the virus contains a lipid bilayer and is a derivative of the nuclear envelope of the host cell; Between the capsid and the outer shell of the virus are matrix proteins; The supercapsid has glycoprotein spikes formed by nuclear membrane proteins. Necessary for the attachment and penetration of viruses into the host cell.

Slide 7

Slide 11
Classification of human herpes viruses (HHV)
Currently, 3 subfamilies have been formed in the Herpesviridae family: Alphaherpesvirinae; Bethaherpesvirinae; Gammaherpesvirinae.

Slide 12
Subfamily Alphaherpesvirinae
Viruses are characterized by a short reproduction cycle with a cytopathic effect in the cells of infected cultures. These include: Herpes simplex virus type 1 (HSV-I); Herpes simplex virus type 2 (HSV-II); Herpes virus type 3 - varicella zoster virus.

Slide 13
Subfamily Bethaherpesvirinae
Viruses are characterized by strictly expressed pathogenicity for one host species. They include: Herpes virus type 5 - human cytomegalovirus (CMV).

Slide 14
Subfamily Gammaherpesvirinae
Viruses are characterized by a strictly expressed tropism for B- or T-lymphocytes, in which they persist for a long time. These include: Herpes virus type 4 - Epstein-Barr virus (EBV); Herpes virus type 6 (HHV - 6); Herpes virus type 7 (HHV - 7); Herpes virus type 8 (HHV - 8) - Herpes virus associated with Kaposi's Sarcoma.

Slide 15
Features of family reproduction
"Stages of herpes virus reproduction." 1 - adsorption of the virus on the cell through interaction of the virus with receptors on the cell membrane; 2 - penetration of the virus into the cell; 3 - virus inside a cell vacuole; 4 - “undressing” of the virus; 5 - replication of viral nucleic acid in the cell nucleus; 6 - synthesis of viral proteins on cell ribosomes; 7 - virus formation; 8 - exit of the virus from the cell by budding.

Slide 17

Slide 19

Slide 20
Stages of herpes
Precursor stage. It begins with a sensation of tingling, itching and burning on the lips. Duration from several hours to 1 day. Hyperemia stage. Literally on the same day as the tingling sensation, swelling and redness of the lip occurs. The condition is usually accompanied by itching and lasts on average 1-2 days. Bubble stage. A group of several bubbles is formed, which merge with each other into one painful bubble filled with lymph. This usually happens on the second day and is accompanied by very painful sensations. Stage of erosion formation. On day 3, the blisters transform into ulcers and pustules, which then form a sore. Usually it is gray in color with a bright red ring around it. The liquid released from the sore contains virus particles in a concentration of 1 million per 1 ml. and is highly contagious

Slide 21
5. Crust formation stage. From days 4 to 9, the sore dries out and crusts over. In this case, the pain becomes less, but severe itching appears. The sore may fall off in parts and bleed. Herpes begins to heal from the inside, the sore becomes smaller. 6. Healing stage. On days 9-11, the wound heals and heals. However, redness may persist for another two days. During this period, the virus returns to a dormant state, in which it can remain until it is activated again by risk factors. Herpes is most contagious at the blistering stage. The crust stage is no longer contagious.

Slide 22
How is herpes transmitted:
Autoinfection. The virus is transmitted from infected areas of the body to uninfected areas. When contacting another person in a kiss. For infection to occur through a kiss, the virus needs 2 conditions: that the carrier has an active phase of herpes (and it can be asymptomatic) that the partner has a predisposition to infection: an abundance of saliva, small wounds. Upon contact with a contaminated surface. The virus is able to survive for some time outside its host: in a humid environment, at a temperature of 37°. That is, it is possible to become infected by drinking from the same glass or using the same lipstick. On plastic surfaces under favorable conditions, the virus survives for about 4 hours.

Slide 1
It is estimated that 22 million people in the country suffer from herpes; annually suffer: at least 3 thousand people - herpetic neuroinfections (10% of encephalitis and 20% of meningoecephalitis - HSV etiology); 300 thousand – 500 thousand – ophthalmoherpes (60% of keratitis – HSV etiology); 8 million people – genital herpes; 10 -12 million people – orofacial herpes. Karazhas N.V., Malinovskaya V.V. – 2011 According to WHO: Mortality from disseminated forms of the disease caused by HSV is 15.8% - second place after influenza; HSV - infection - 35.8% - among diseases of viral etiology; 60–90% of the population at different periods of life are infected with one or more types of viruses, 50% of them experience relapses of the disease. http://prezentacija.biz/Slide 2
 Classification of the International Committee on Taxonomy of Viruses (1995) Human herpes viruses Herpes humanum virus HHV-I - Herpes simplex virus 1 - HSV-1 HHV-II - Herpes simplex virus 2 - HSV-2 HHV-III - Varicella-Zoster virus - VZV - 3 HHV-IV -Epstein-Barr virus -EBV – 4 HHV-V - Cytomegalovirus -CMV – 5 HHV-VI -Human herpes virus type 6 -HHV – 6 HHV-VII -Chronic fatigue virus -HHV – 7 HHV-VIII - Kaposi's sarcoma associated virus - HHV-8
Classification of the International Committee on Taxonomy of Viruses (1995) Human herpes viruses Herpes humanum virus HHV-I - Herpes simplex virus 1 - HSV-1 HHV-II - Herpes simplex virus 2 - HSV-2 HHV-III - Varicella-Zoster virus - VZV - 3 HHV-IV -Epstein-Barr virus -EBV – 4 HHV-V - Cytomegalovirus -CMV – 5 HHV-VI -Human herpes virus type 6 -HHV – 6 HHV-VII -Chronic fatigue virus -HHV – 7 HHV-VIII - Kaposi's sarcoma associated virus - HHV-8
Slide 3
 Phylogenetic classification of human herpesviruses Alpha viruses (HSV-1, 2 and VZV). They are characterized by rapid replication (4-8 hours), the ability to undergo cytolysis and asymptomatic persistence in neutron cells. Beta viruses (CMV, HHV-6 and HHV-7). They replicate slowly, cause cytomegalic transformation of cells, and the main foci of latency are monocytes and their precursors, endothelial cells of the microvasculature, alveolar macrophages, T-lymphocytes and bone marrow stromal cells. Gamma viruses (EBV and HHV-8). Transforming human viruses that promote the development of malignant cell transformation. Persisting for life in B-lymphocytes or being in a latent state, they have the ability to malignize them.
Phylogenetic classification of human herpesviruses Alpha viruses (HSV-1, 2 and VZV). They are characterized by rapid replication (4-8 hours), the ability to undergo cytolysis and asymptomatic persistence in neutron cells. Beta viruses (CMV, HHV-6 and HHV-7). They replicate slowly, cause cytomegalic transformation of cells, and the main foci of latency are monocytes and their precursors, endothelial cells of the microvasculature, alveolar macrophages, T-lymphocytes and bone marrow stromal cells. Gamma viruses (EBV and HHV-8). Transforming human viruses that promote the development of malignant cell transformation. Persisting for life in B-lymphocytes or being in a latent state, they have the ability to malignize them.
Slide 4
 Forms of interaction of herpes viruses with the host organism. 1. Acute form - a short incubation period followed by the development of a characteristic clinical picture of the disease and the reverse dynamics of symptoms; 2. Chronic form – clinical and laboratory symptoms of the disease appear over a long period of time (more than 6 months); 3. Inapparent (asymptomatic) form, when clinical symptoms of the disease are not expressed, and the infection is documented laboratory (virological and serological research methods); 4. The form of a slow viral infection is a long incubation period (months and years) followed by a slow progressive course, with the development of severe clinical symptoms and, ultimately, the death of the patient.
Forms of interaction of herpes viruses with the host organism. 1. Acute form - a short incubation period followed by the development of a characteristic clinical picture of the disease and the reverse dynamics of symptoms; 2. Chronic form – clinical and laboratory symptoms of the disease appear over a long period of time (more than 6 months); 3. Inapparent (asymptomatic) form, when clinical symptoms of the disease are not expressed, and the infection is documented laboratory (virological and serological research methods); 4. The form of a slow viral infection is a long incubation period (months and years) followed by a slow progressive course, with the development of severe clinical symptoms and, ultimately, the death of the patient.
Slide 5
 Persistence of herpes viruses is a continuous and cyclical reproduction (replication) of the virus in infected cells of tropic tissues, which is the cause of the development of the infectious process. Latency of herpes viruses does not manifest itself clinically, but is diagnosed only in the presence of specific Ig G against the virus (seropositivity) in low titers, and the virus itself is not detected in peripheral blood during this period (by PCR). In a state of latency, the full cycle of virus reproduction is disrupted, and it is found in the host cells in the form of subviral structures in the cell nucleus.
Persistence of herpes viruses is a continuous and cyclical reproduction (replication) of the virus in infected cells of tropic tissues, which is the cause of the development of the infectious process. Latency of herpes viruses does not manifest itself clinically, but is diagnosed only in the presence of specific Ig G against the virus (seropositivity) in low titers, and the virus itself is not detected in peripheral blood during this period (by PCR). In a state of latency, the full cycle of virus reproduction is disrupted, and it is found in the host cells in the form of subviral structures in the cell nucleus.
Slide 6
 Risk factors for the occurrence of herpesvirus infections Cooling Solar insolation UV irradiation Being in conditions of sharp temperature fluctuations Emotional stress Mental disorders Physical overexertion Sudden changes in climatic zones Constant lack of sleep Fasting Excessive alcohol consumption
Risk factors for the occurrence of herpesvirus infections Cooling Solar insolation UV irradiation Being in conditions of sharp temperature fluctuations Emotional stress Mental disorders Physical overexertion Sudden changes in climatic zones Constant lack of sleep Fasting Excessive alcohol consumption
Slide 7
 The first description of the symptoms of a “cold” on the lips, accompanied by fever, was made by the Roman physician Herodotus in the 5th century BC. The word herpes comes from the ancient Greek - herpain (ερπυσμός) or creeping. This is how Hippocrates dubbed this disease 2400 years ago. Hippocrates Herodotus Avicenna Paracelsus
The first description of the symptoms of a “cold” on the lips, accompanied by fever, was made by the Roman physician Herodotus in the 5th century BC. The word herpes comes from the ancient Greek - herpain (ερπυσμός) or creeping. This is how Hippocrates dubbed this disease 2400 years ago. Hippocrates Herodotus Avicenna Paracelsus
Slide 8
 The source of infection is patients with various forms of the disease and virus carriers. Routes of transmission of the virus: airborne droplets sexual vertical contact household parenteral Virus transmission factors: blood saliva urine vesicular and vaginal secretions sperm
The source of infection is patients with various forms of the disease and virus carriers. Routes of transmission of the virus: airborne droplets sexual vertical contact household parenteral Virus transmission factors: blood saliva urine vesicular and vaginal secretions sperm
Slide 9
 Clinical manifestations of HSV infection according to ICD-10. B00. Infections caused by the herpes virus (herpes simplex). B00.0. Herpetic eczema. B00.1. Herpetic vesicular dermatitis. B00.2. Herpetic gingivostomatitis and pharyngotonsillitis. B00.3. Herpetic meningitis B00.4. Herpetic encephalitis B00.5. Herpetic eye disease. B00.7. Disseminated herpetic disease B00.8. Other forms of herpetic infections B00.9 Herpetic infection, unspecified. A60. Anogenital herpetic viral infection(herpes simplex). A60.0. Herpetic infections of the genital organs and genitourinary tract. A60.1. Herpetic infections of the perianal skin and rectum. A60.9. Anogenital herpetic infection, unspecified.
Clinical manifestations of HSV infection according to ICD-10. B00. Infections caused by the herpes virus (herpes simplex). B00.0. Herpetic eczema. B00.1. Herpetic vesicular dermatitis. B00.2. Herpetic gingivostomatitis and pharyngotonsillitis. B00.3. Herpetic meningitis B00.4. Herpetic encephalitis B00.5. Herpetic eye disease. B00.7. Disseminated herpetic disease B00.8. Other forms of herpetic infections B00.9 Herpetic infection, unspecified. A60. Anogenital herpetic viral infection(herpes simplex). A60.0. Herpetic infections of the genital organs and genitourinary tract. A60.1. Herpetic infections of the perianal skin and rectum. A60.9. Anogenital herpetic infection, unspecified.
Slide 10

Slide 11
 Herpes Simplex of the mucous membranes and skin Damage to the eyes, mouth and skin Herpetic stomatitis
Herpes Simplex of the mucous membranes and skin Damage to the eyes, mouth and skin Herpetic stomatitis
Slide 12

Slide 13

Slide 14

Slide 15

Slide 16

Slide 17

Slide 18
 Detection of antibodies to HSV - ELISA Important to know: antibodies to HSV are detected in 90 - 97% of those examined who do not have clinical symptoms of GI. An increase in antibody titers to HSV occurs late, several weeks after infection or reactivation of the virus, and may not be observed in patients with IDS. The AT titer does not always correspond to the clinical manifestations of the infection: in some asymptomatic carriers, high AT titers are detected, while in some patients with severe symptoms, AT titers remain low. Class M antibodies are an indicator of active infection after primary infection and are detected in the blood for several months or years. It is advisable to examine paired sera (interval 7-10 days). A 4-fold increase in antibodies to HSV of the IgG class is an indicator of active infection.
Detection of antibodies to HSV - ELISA Important to know: antibodies to HSV are detected in 90 - 97% of those examined who do not have clinical symptoms of GI. An increase in antibody titers to HSV occurs late, several weeks after infection or reactivation of the virus, and may not be observed in patients with IDS. The AT titer does not always correspond to the clinical manifestations of the infection: in some asymptomatic carriers, high AT titers are detected, while in some patients with severe symptoms, AT titers remain low. Class M antibodies are an indicator of active infection after primary infection and are detected in the blood for several months or years. It is advisable to examine paired sera (interval 7-10 days). A 4-fold increase in antibodies to HSV of the IgG class is an indicator of active infection.
Slide 19
 Virological method for detecting HSV in cell culture + The most sensitive and specific Detection of the CPD of the virus in a cell culture on days 1–2 correlates with a pronounced infectious process (primary infection or early stage of recurrent infection) Detection of the CPD of the virus in a cell culture after 2–3 passages is typical for sluggish infectious process or for asymptomatic infection It is a reference method in assessing the effectiveness of antiviral treatment - The disadvantage of the method is the need to obtain a cell culture, which is not always possible for technical reasons. Section of an infected human embryonic fibroblast cell (virions in the cell nucleus)
Virological method for detecting HSV in cell culture + The most sensitive and specific Detection of the CPD of the virus in a cell culture on days 1–2 correlates with a pronounced infectious process (primary infection or early stage of recurrent infection) Detection of the CPD of the virus in a cell culture after 2–3 passages is typical for sluggish infectious process or for asymptomatic infection It is a reference method in assessing the effectiveness of antiviral treatment - The disadvantage of the method is the need to obtain a cell culture, which is not always possible for technical reasons. Section of an infected human embryonic fibroblast cell (virions in the cell nucleus)
Slide 20
 Cytomorphological method - light microscopy of biological material after staining on a glass slide (according to Romanovsky - Giemsa, Papanicol, according to Seller - Pavlovsky, etc.). During GI, giant cells and intranuclear inclusions are detected. “+” method is fast and cheap “-” does not allow to differentiate changes caused by HSV and other GIs. sensitivity only 60%
Cytomorphological method - light microscopy of biological material after staining on a glass slide (according to Romanovsky - Giemsa, Papanicol, according to Seller - Pavlovsky, etc.). During GI, giant cells and intranuclear inclusions are detected. “+” method is fast and cheap “-” does not allow to differentiate changes caused by HSV and other GIs. sensitivity only 60%
Slide 21
 Detection of HSV DNA in PCR is a method of molecular biology that allows, using repeated cycles of amplification (copying), to obtain large quantity copies of DNA in biological material.
Detection of HSV DNA in PCR is a method of molecular biology that allows, using repeated cycles of amplification (copying), to obtain large quantity copies of DNA in biological material.
Slide 22
 “+” The sensitivity and specificity of PCR reaches 90–95%. A very small amount of material is sufficient. Results are ready in 1–2 days “-” The method sometimes gives false-positive results. The presence of a relationship between mortality in newborns and viremia caused by HSV-1 and HSV-2 recommends using this method for laboratory screening for generalized HI among high-risk children.
“+” The sensitivity and specificity of PCR reaches 90–95%. A very small amount of material is sufficient. Results are ready in 1–2 days “-” The method sometimes gives false-positive results. The presence of a relationship between mortality in newborns and viremia caused by HSV-1 and HSV-2 recommends using this method for laboratory screening for generalized HI among high-risk children.
Slide 23
 Methods for detecting HSV antigens (NRIF and RIF) Material for research - contents of vesicles, scrapings from the bottom of erosion, urethral mucosa, vaginal walls, cervical canal, eye conjunctiva, blood cells. Smears are treated with a fluorescent preparation and viewed under a fluorescent microscope (+ a smear containing at least 3 morphologically altered epithelial cells with intense fluorescence and localization typical of HSV in the nucleus or in the nucleus and cytoplasm at the same time). Neurons affected by H. simplex Immunofluorescence staining reveals viral antigens
Methods for detecting HSV antigens (NRIF and RIF) Material for research - contents of vesicles, scrapings from the bottom of erosion, urethral mucosa, vaginal walls, cervical canal, eye conjunctiva, blood cells. Smears are treated with a fluorescent preparation and viewed under a fluorescent microscope (+ a smear containing at least 3 morphologically altered epithelial cells with intense fluorescence and localization typical of HSV in the nucleus or in the nucleus and cytoplasm at the same time). Neurons affected by H. simplex Immunofluorescence staining reveals viral antigens
Slide 24
 Specific vaccination against HSV infection The St. Petersburg vaccine is produced on chicken fibroblast cells, the Moscow one - "Vitagerpavak" - on the "Vero:B" cell line standardized in world practice, is more immunogenic, contains specific antigens of the herpes virus types 1 and 2, which stimulate cellular mechanisms of resistance, restoring the functional activity of blood lymphocytes, as well as ensuring high activity of NK-1 cells (normal killer cells). Release form The vaccine is produced in 5 ml bottles of 0.3 ml each. One vaccination dose is 0.2 ml. The box contains 5 bottles and instructions for use. Directions for use and dosage. Vaccination is carried out in medical institutions (hospital, dispensary, clinic) under the supervision of a doctor. The vaccine is used in the remission stage, no earlier than 5 days after the complete disappearance of clinical manifestations of herpetic infection. The drug is administered intradermally into the area of the inner surface of the forearm using a syringe in a single dose of 0.2 ml (control - formation of a “lemon peel”). The course of vaccination for herpes infection of the skin and mucous membranes consists of 5 injections, which are carried out with an interval of 7 days - 10 days (depending on the severity of the disease). For patients with complicated herpes infection, the 2nd and subsequent injections are repeated at intervals of 10 days. After 6 months, a second course of vaccination is carried out (5 injections).
Specific vaccination against HSV infection The St. Petersburg vaccine is produced on chicken fibroblast cells, the Moscow one - "Vitagerpavak" - on the "Vero:B" cell line standardized in world practice, is more immunogenic, contains specific antigens of the herpes virus types 1 and 2, which stimulate cellular mechanisms of resistance, restoring the functional activity of blood lymphocytes, as well as ensuring high activity of NK-1 cells (normal killer cells). Release form The vaccine is produced in 5 ml bottles of 0.3 ml each. One vaccination dose is 0.2 ml. The box contains 5 bottles and instructions for use. Directions for use and dosage. Vaccination is carried out in medical institutions (hospital, dispensary, clinic) under the supervision of a doctor. The vaccine is used in the remission stage, no earlier than 5 days after the complete disappearance of clinical manifestations of herpetic infection. The drug is administered intradermally into the area of the inner surface of the forearm using a syringe in a single dose of 0.2 ml (control - formation of a “lemon peel”). The course of vaccination for herpes infection of the skin and mucous membranes consists of 5 injections, which are carried out with an interval of 7 days - 10 days (depending on the severity of the disease). For patients with complicated herpes infection, the 2nd and subsequent injections are repeated at intervals of 10 days. After 6 months, a second course of vaccination is carried out (5 injections).
Slide 25
 Clinical forms of diseases caused by herpes viruses (continued) Virus Primary infection Reactivation after latency Human herpes virus type 4 - HHV-4 - Epstein-Barr virus - EBV - EBV Infectious mononucleosis Muscle sarcoma Encephalitis in newborns Lymphoid interstitial pneumonia in children Infectious mononucleosis Hepatitis Burkitt's lymphoma Nasopharyngeal carcinoma Hairy leukoplakia of the tongue EBV-associated lymphoproliferative syndrome B-cell lymphoma Chronic fatigue and immune depression syndrome Autoimmune pathology Human herpes virus type 5 - HHV-5-cytomegalovirus- CMV-СMV Heterophilic-negative mononucleosis Vasculitis Neonatal CMV infection Subclinical infection Heterophilic negative mononucleosis CMV-retinitis CMV-hepatitis CMV-pneumonia CMV-encephalitis CMV-colitis/cholangitis CMV-adrenal insufficiency Transplant rejection reaction Atherosclerosis Simian herpes virus B Lethal encephalomyelitis when infected in humans
Clinical forms of diseases caused by herpes viruses (continued) Virus Primary infection Reactivation after latency Human herpes virus type 4 - HHV-4 - Epstein-Barr virus - EBV - EBV Infectious mononucleosis Muscle sarcoma Encephalitis in newborns Lymphoid interstitial pneumonia in children Infectious mononucleosis Hepatitis Burkitt's lymphoma Nasopharyngeal carcinoma Hairy leukoplakia of the tongue EBV-associated lymphoproliferative syndrome B-cell lymphoma Chronic fatigue and immune depression syndrome Autoimmune pathology Human herpes virus type 5 - HHV-5-cytomegalovirus- CMV-СMV Heterophilic-negative mononucleosis Vasculitis Neonatal CMV infection Subclinical infection Heterophilic negative mononucleosis CMV-retinitis CMV-hepatitis CMV-pneumonia CMV-encephalitis CMV-colitis/cholangitis CMV-adrenal insufficiency Transplant rejection reaction Atherosclerosis Simian herpes virus B Lethal encephalomyelitis when infected in humans
Slide 26
 By definition, infectious mononucleosis is an acute viral disease characterized by: fever, enlarged lymph nodes, hepato- and splenomegaly, the appearance of atypical mononuclear cells and heterophilic antibodies in the blood.
By definition, infectious mononucleosis is an acute viral disease characterized by: fever, enlarged lymph nodes, hepato- and splenomegaly, the appearance of atypical mononuclear cells and heterophilic antibodies in the blood.
Slide 27
 In the International Statistical Classification of Diseases and Related Health Problems, tenth revision (ICD-10), MI is included in category B 27. The concept of MI includes synonyms: glandular fever, monocytic tonsillitis, Pfeiffer's disease, which previously existed. Further, according to etiology, there are: B 27.0 Mononucleosis caused by the gammaherpetic virus. Mononucleosis caused by Epstein-Barr virus B 27.1 Cytomegalovirus mononucleosis B 27.8 Other infectious mononucleosis B 27.9 Infectious mononucleosis, unspecified. (WHO. Geneva, 1995)
In the International Statistical Classification of Diseases and Related Health Problems, tenth revision (ICD-10), MI is included in category B 27. The concept of MI includes synonyms: glandular fever, monocytic tonsillitis, Pfeiffer's disease, which previously existed. Further, according to etiology, there are: B 27.0 Mononucleosis caused by the gammaherpetic virus. Mononucleosis caused by Epstein-Barr virus B 27.1 Cytomegalovirus mononucleosis B 27.8 Other infectious mononucleosis B 27.9 Infectious mononucleosis, unspecified. (WHO. Geneva, 1995)
Slide 28
 - many modern researchers believe that CMV mononucleosis often occurs after blood transfusions and is observed in older children and pregnant women due to reactivation of the latent virus. (Belozerov E.S. - 2005; Granitov V.M. - 2001; Dolgushina M.V. - 2004; Kisteneva L.B., Cheshik S.G. - 2004; Prilutsky A.S. . – 2002) foreign authors describe CMV mononucleosis in adolescents, children and even newborns. (Lui, W.Y - 1972, Pannuti, C.S. et al - 1982, Ralph D. Feigin et al - 1998) The first reports of CMV mononucleosis appeared in the UK in 1965-1966. in the works of S. Lamb, E. Klemola, L. Kaariainen.
- many modern researchers believe that CMV mononucleosis often occurs after blood transfusions and is observed in older children and pregnant women due to reactivation of the latent virus. (Belozerov E.S. - 2005; Granitov V.M. - 2001; Dolgushina M.V. - 2004; Kisteneva L.B., Cheshik S.G. - 2004; Prilutsky A.S. . – 2002) foreign authors describe CMV mononucleosis in adolescents, children and even newborns. (Lui, W.Y - 1972, Pannuti, C.S. et al - 1982, Ralph D. Feigin et al - 1998) The first reports of CMV mononucleosis appeared in the UK in 1965-1966. in the works of S. Lamb, E. Klemola, L. Kaariainen.
Slide 29
 - this is one of the clinical variants of the acute phase of a typical CMV infection in an immunocompetent person (in another variant, primary CMV infection is asymptomatic). - or a consequence of reactivation of infection in immunosuppressed patients. Cytomegalovirus mononucleosis (Granitov V.M. - 2001; Samokhin P.A. - 1987; Chuchalin A.G. - 2006; King K. Holmes et al - 1999; Ralpf D. Feigin - 1998 .)
- this is one of the clinical variants of the acute phase of a typical CMV infection in an immunocompetent person (in another variant, primary CMV infection is asymptomatic). - or a consequence of reactivation of infection in immunosuppressed patients. Cytomegalovirus mononucleosis (Granitov V.M. - 2001; Samokhin P.A. - 1987; Chuchalin A.G. - 2006; King K. Holmes et al - 1999; Ralpf D. Feigin - 1998 .)
Slide 30

Slide 31
 Clinical forms of diseases caused by herpes viruses (continued) Virus Primary infection Reactivation after latency Human herpes virus type 6 - HHV-6-HHV-6 Sudden exanthema in children Heterophilic-negative mononucleosis Vasculitis Heterophilic-negative mononucleosis Hepatitis Lymphoproliferative diseases Interstitial pneumonia in people with immunodeficiency Encephalitis Malignant neoplasms Chronic fatigue syndrome and immune depression Autoimmune pathology Psychosis Human herpes virus type 7 - HHV-7-HHV-7 Possible exanthema in children Chronic fatigue syndrome and immune depression Diseases of the skin and central nervous system of an autoimmune nature. Stomach cancer Human herpes virus type 8 - HHV-8 - HHV-8 Not known Kaposi's sarcoma Non-Hodgkin's B - lymphoma Lymphoproliferative disease - Castleman's disease
Clinical forms of diseases caused by herpes viruses (continued) Virus Primary infection Reactivation after latency Human herpes virus type 6 - HHV-6-HHV-6 Sudden exanthema in children Heterophilic-negative mononucleosis Vasculitis Heterophilic-negative mononucleosis Hepatitis Lymphoproliferative diseases Interstitial pneumonia in people with immunodeficiency Encephalitis Malignant neoplasms Chronic fatigue syndrome and immune depression Autoimmune pathology Psychosis Human herpes virus type 7 - HHV-7-HHV-7 Possible exanthema in children Chronic fatigue syndrome and immune depression Diseases of the skin and central nervous system of an autoimmune nature. Stomach cancer Human herpes virus type 8 - HHV-8 - HHV-8 Not known Kaposi's sarcoma Non-Hodgkin's B - lymphoma Lymphoproliferative disease - Castleman's disease
Slide 32

Slide 33

Slide 34

Slide 35
 PATHOGENESIS OF INFECTIOUS MONONUCLEOSIS PRIMARY REPLICATION OF THE VIRUS IN THE EPITHELIA OF THE ORO-NASPHARYNGE and penetration into B-lymphocytes (EBV) and T-lymphocytes (CMV and HHV-6) LYMPHORETICULAR SYSTEM - DISSEMINATION OF THE CAPACITOR REPLICATION VIRUS WITH DNA INTEGRATION INTO THE CELL GENOME ENLARGEMENT OF LYMPH NODES, NASOPHARYNX TONSILS, TONSILOPHARYNGITIS, HEPATO-, SPLENOMEGALY, ATYPICAL MONONUCLEARS (B and T LYMPHOCYTES)
PATHOGENESIS OF INFECTIOUS MONONUCLEOSIS PRIMARY REPLICATION OF THE VIRUS IN THE EPITHELIA OF THE ORO-NASPHARYNGE and penetration into B-lymphocytes (EBV) and T-lymphocytes (CMV and HHV-6) LYMPHORETICULAR SYSTEM - DISSEMINATION OF THE CAPACITOR REPLICATION VIRUS WITH DNA INTEGRATION INTO THE CELL GENOME ENLARGEMENT OF LYMPH NODES, NASOPHARYNX TONSILS, TONSILOPHARYNGITIS, HEPATO-, SPLENOMEGALY, ATYPICAL MONONUCLEARS (B and T LYMPHOCYTES)
Slide 36
 Diagnosis of infectious mononucleosis in children O- determination of heterophilic antibodies in the blood O- determination of antibodies to viruses in the blood O- determination of viral DNA in biological media P- determination of viral antigens in blood leukocytes (lymphocytes and macrophages)
Diagnosis of infectious mononucleosis in children O- determination of heterophilic antibodies in the blood O- determination of antibodies to viruses in the blood O- determination of viral DNA in biological media P- determination of viral antigens in blood leukocytes (lymphocytes and macrophages)
Slide 37
 Structure of EBV DNA Epstein-Barr virus CAPSIDS (VCA) anti-VCA IgM anti-VCA IgG ENVIRONMENT ANTIGENS (EA,gp350/220) anti-EA IgM anti-EA IgG NUCLEOCAPSID (EBNA) anti EBNA IgM,IgG
Structure of EBV DNA Epstein-Barr virus CAPSIDS (VCA) anti-VCA IgM anti-VCA IgG ENVIRONMENT ANTIGENS (EA,gp350/220) anti-EA IgM anti-EA IgG NUCLEOCAPSID (EBNA) anti EBNA IgM,IgG
Slide 38
 Dynamics of the production of antibodies to various groups of immunogenic proteins of EBV in the human body 1 0 2 3 4 2 3 4 5 w eeks M onths IgG-VCA IgM-VCA IgG-EA IgM-EA IgG-NA-1
Dynamics of the production of antibodies to various groups of immunogenic proteins of EBV in the human body 1 0 2 3 4 2 3 4 5 w eeks M onths IgG-VCA IgM-VCA IgG-EA IgM-EA IgG-NA-1
Slide 39

Slide 40
 Interpretation of serological data for EBV infection Stage of infection EA VCA NA IgM IgG IgM IgG IgG Incubation period or absence of infection _ _ _ _ _ Very early primary infection _ + _ _ Early primary infection + + + + + Late primary infection + + + + + Atypical primary infection + + _ _ + Chronic infection + + + + _ Early past infection _ + _ + + Late past infection (latent infection in clinically healthy individuals) _ _ _ + + Reactivation + + + + + Atypical reactivation + + _ _ +
Interpretation of serological data for EBV infection Stage of infection EA VCA NA IgM IgG IgM IgG IgG Incubation period or absence of infection _ _ _ _ _ Very early primary infection _ + _ _ Early primary infection + + + + + Late primary infection + + + + + Atypical primary infection + + _ _ + Chronic infection + + + + _ Early past infection _ + _ + + Late past infection (latent infection in clinically healthy individuals) _ _ _ + + Reactivation + + + + + Atypical reactivation + + _ _ +
The herpes virus is a silent cohabitant of our body. Herpes is a fine blistering rash, most often on
lips or nose, popularly called "fever", or
"a cold." The name "herpes" comes from
the ancient Greek word "herpein" ("to crawl"). This
characteristic property of herpes: from a single small
bubble spread throughout the body.
“Bad news in a protein shell” by P. Medawar
Herpes viruses can be present in the human body withnormal immune system is asymptomatic, and in people with
immunosuppression causes severe diseases with
fatal.
Once the herpes virus enters the body, it remains there
forever.
According to WHO:
Herpes is one of the most commonhuman viral infections.
95% of the world's people are infected with the virus
herpes simplex (HSV)
up to 20% of them have some kind of active
clinical manifestations of infection.
Mortality from herpetic infections among
viral diseases are in second place
(15.8%) after hepatitis (35.8%);
The incidence of herpes on the lips varies from
person to person and can be repeated from 2 to 12
once a year.
Epidemiology of the herpes virus
Epidemiological studies show that herpesdistributed everywhere.
Humoral immune response is accompanied by
mainly by the production of antibodies to antigens.
Serological reactions in which the antigen is
the virus itself is used - complement fixation reactions,
neutralization, indirect hemagglutination, method
indirect immunofluorescence,
RIA and ELISA - do not allow you to determine what type
Herpes virus is caused by infection.
Herpes simplex virus type 1 is acquired earlier and
more often than herpes simplex virus type 2. Antibodies to
More than 90% of people have herpes simplex virus type 1
over 40 years old.
The structure of the herpes virus
DNA virus;Viral capsid in the form
The icosahedron consists of 162
capsomeres;
Diameter of the outer shell of the virus
– 180 nm, viral nucleocapsid
– 100 nm.
Outer shell of the virus
contains a double layer of lipids and
is a derivative
nuclear envelope of the host cell;
Between the capsid and the outer
the virus shell contains proteins
matrix;
Supercapsid has
glycoprotein spikes,
formed by nuclear proteins
membranes. Essential for
attachment and penetration
viruses into the host cell. Herpesvirus
Classification of human herpes viruses (HHV)
Currently in the familyHerpesviridae formed 3
subfamilies:
Alphaherpesvirinae;
Bethaherpesvirinae;
Gammaherpesvirinae.
Subfamily Alphaherpesvirinae
Viruses are characterized by a short reproduction cycle withcytopathic effect in infected cells
crops These include:
Herpes simplex virus type 1 (HSV-I);
Herpes simplex virus type 2 (HSV-II);
Herpes virus type 3 - varicella zoster virus.
Subfamily Bethaherpesvirinae
Viruses are characterized by strictly expressedpathogenicity for one host species. They include:
Herpes virus type 5 is human cytomegalovirus (HCMV).
Subfamily Gammaherpesvirinae
Viruses are characterized by strictly expressedtropism for B- or T-lymphocytes, in which they
persist for a long time. These include:
Herpes virus type 4 - Epstein-Barr virus (EBV);
Herpes virus type 6 (HHV - 6);
Herpes virus type 7 (HHV - 7);
Herpes virus type 8 (HHV - 8) - Herpes virus,
associated with Kaposi's Sarcoma.
Features of family reproduction
"Stages of herpes virus reproduction."1 - adsorption of the virus on the cell by interaction
a virus with receptors on the cell membrane;
2 - penetration of the virus into the cell;
3 - virus inside a cell vacuole;
4 - “undressing” of the virus;
5 - replication of viral nucleic acid in the nucleus
cells;
6 - synthesis of viral proteins on cell ribosomes;
7 - virus formation;
8 - exit of the virus from the cell by budding. The mechanism of reproduction of the herpes virus
Development of the herpes virus over time
Stages of herpes
1.Precursor stage. Starts with a tingling sensationitching and burning on the lips. Duration from several
hours to 1 day.
2. Stage of hyperemia. Literally on the same day as
tingling occurs swelling and redness of the lips. State
usually accompanied by itching and lasts on average 1-2 days.
3. Bubbles stage. A group of several is formed
bubbles that merge into one
painful lymph-filled bladder. Usually this
occurs on the second day and is accompanied by very
painful sensations.
4. Stage of erosion formation. On day 3 bubbles
transform into ulcers and pustules, which then
form a sore. Usually it's gray, I'm bright red
ring around. The fluid released from the sore contains
virus particles in a concentration of 1 million per 1 ml. and is
especially contagious 5.
6.
Crust formation stage. From 4 to 9 days sore
dries out and becomes crusty. At the same time the pain
becomes smaller, but severe itching appears. Sore
may fall off in parts and bleed. Herpes
begins to heal from the inside, the sore becomes smaller.
Healing stage. Occurs on days 9-11
wound healing and healing. Nevertheless
redness may persist for another two days. In that
period, the virus returns to a dormant state, in
which may remain until it is again
activated under the influence of risk factors.
Herpes is most contagious at the blistering stage.
The crust stage is no longer contagious.
How is herpes transmitted:
Autoinfection. The virus is transmitted from infected peopleareas of the body to uninfected ones.
When contacting another person in a kiss. To
infection occurred through a kiss, the virus needs 2
conditions:
1. so that the carrier has an active phase of herpes (moreover, it
may be asymptomatic)
2.so that the partner has a predisposition to infection:
an abundance of saliva, small wounds.
. Upon contact with a contaminated surface. The virus is capable
survive for some time outside its carrier: in damp
environment, at a temperature of 37°. That is, it is possible to become infected
when drinking from the same glass, using the same lipstick.
On plastic surfaces under favorable conditions
The virus survives for about 4 hours. The source of infection is a sick person and
virus carrier.
The virus is transmitted mainly by airborne droplets and
by contact.
The largest number of cases is registered in
cold months, but as a rule there are no epidemics.
*H*H herpes infection (synonym: herpes simplex) is a collective name for infections caused by herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2). *T*T The term “herpes” (from the Greek herpes - creeping) was used by Herodotus in 100 BC to describe blisters accompanied by fever.

* The first type is Herpes Labialis (labial form of herpes), HSV-1, which affects the face, nasolabial triangle, oral cavity, nasal cavity, and sometimes the cheeks. * The second type is genital herpes - HSV-2. * The third type is herpes zoster, official name: chickenpox virus - shingles or chickenpox - Herpes Zoster * The fourth type is the Epstein-Barr virus

The fifth type is cytomegalovirus (cyto - cell, megalo - large). The sixth type is divided into two variants: type six "A" is associated today with various lymphoproliferative diseases (i.e., associated with the proliferation of cells - tumors, for example), of a rather severe nature, such as hemocytoblastosis, lymphoma, lymphosarcoma, and so on; type six "B" is associated with sudden exanthema (fine-grained rash). The seventh type is assumed to be one of the main etiopathogens of chronic fatigue syndrome. The eighth type is the etiopathogen of Kaposi's sarcoma in AIDS.

* When infected, the herpes virus integrates into a human cell, changes its genetic apparatus and, using its enzymatic apparatus, switches the cell to the synthesis of its mature viral particles - virions, which in turn infect more and more new cells of the body in an avalanche-like manner, which leads to the development of herpes diseases. * The virus can also infect blood cells - these include red blood cells, erythrocytes, and lymphocytes.


* HSV enters the human body through damaged skin and mucous membranes. * Phase 1 - the virus invades epithelial cells (oral mucosa, pharynx or genital organs), where it multiplies. * Phase 2 - penetrates the sensory nerve endings and along the centripetal nerve fibers into the paravertebral ganglia. * Phase 3 - resolution of the primary disease and elimination of HSV from tissues and organs * Phase 4 - reactivation of HSV reproduction and its movement along nerve fibers to the site of primary entry (gate of infection) with relapse of a specific infectious-inflammatory process and possible dissemination of the infection.


* Classification of herpetic infection According to the mechanism of infection * 1. Acquired: * primary * recurrent (secondary) * 2. Congenital (intrauterine infection) According to the form of the infectious process * 1. Latent asymptomatic carriage * 2. Localized * 3. Common * 4. Generalized (visceral, disseminated) By localization of lesions * 1. Skin: herpes simplex, eczema herpetiformis, ulcerative necrotizing herpes, zosteriform herpes * 2. Mucous membranes of the oral cavity and oropharynx: stomatitis, gingivitis, pharyngitis, tonsillitis * 3. Upper respiratory tract: acute respiratory disease * 4. Eyes: keratitis, keratoconjunctivitis, iritis, iridocyclitis * 5. Urogenital organs: urethritis, cystitis, vulvovaginitis, cervicitis * 6. Nervous system: meningitis, encephalitis, meningoencephalitis * 7. Internal organs: esophagitis, pneumonia, hepatitis , glomerulonephritis According to the severity of the disease * 1. Mild * 2. Moderate * 3. Severe

* With herpes simplex, the skin of the face is most often affected in the area of the lips (herpes labialis) and the wings of the nose (herpes nasalis). * The typical form of herpes simplex of the skin is characterized by the formation of grouped papules on edematous-hyperemic skin, turning into vesicles with serous contents.


* Stomatitis, gingivitis, pharyngitis and tonsillitis are the most common manifestations of primary infection caused by HSV-1, and are more common in children and young people * Clinical differential diagnosis of herpetic lesions of the mucous membranes from other diseases presents certain difficulties

Clinical diagnosis Variants of the disease Herpetic dermatitis of the eyelids, blepharitis, blepharoconjunctivitis Herpetic conjunctivitis Herpetic keratitis epithelial Tree-like (vesicular, punctate, stellate); Tree-like with stromal lesions; Card-shaped. Herpetic stromal keratitis Herpetic ulcer of the cornea; Discoid keratitis; Herpetic endothelial keratitis; Herpetic keratitis with ulceration; Herpetic keratouveitis without ulceration. Herpetic uveitis Herpetic iritis; Herpetic iridocyclitis; Herpetic neuritis. Postherpetic keratopathy Epithelial; Bullous Clinical classification of herpes viral eye lesions

* Genital herpes (GG) is one of the most common and clinically significant forms of herpes infection. According to approximate data, the number of visits to doctors of various specialties (gynecologists, urologists, dermatologists) in Russia is no more than 15% of the actual incidence of the disease, and total number There may be about 8 million people suffering from various forms of genital herpes in the country.


* The risk of infection largely depends on the following factors: * 1) the duration of the anhydrous period (ascending route of infection due to premature rupture of membranes); * 2) the use of instrumental interventions during childbirth, leading to trauma to the birth canal of the mother and the skin of the newborn; * 3) the level of maternal antibodies that have passed transplacentally to the fetus, and local antibodies that bind the virus in the genital tract.

* Among born children, the number of people infected with the herpes simplex virus ranges from 1:3000 to 1:20000 Clinical forms of neonatal herpes: Clinical forms Frequency of detection, % Mortality Without treatment When using acyclovir intravenously Local form with damage to the skin and mucous membranes 4518 With damage to the central nervous system ( encephalitis) 3556 Disseminated form 2590


* With intranatal and early neonatal infection, two variants of the course of herpetic encephalitis in newborns are distinguished: * 1) diffuse, against the background of a generalized herpetic infection; * 2) focal, without clear symptoms of damage to other visceral organs


* 1) virological methods for the detection and identification of herpes simplex viruses; * 2) methods for detecting antigens of herpes simplex viruses - immunofluorescence and enzyme immunoassay; * 3) polymerase chain reaction (PCR method); * 4) cytomorphological methods; * 5) detection of antibodies using ELISA (enzyme-linked immunosorbent assay); * 6) methods of research and assessment of immune status.


6th year, LF, 42 gr. Most
widespread
persistent infection
is a simple virus
herpes.
About 90% are infected with it
urban population of all
countries of the world, and relapse
the disease is observed in 2–
12% of cases. Over the last 10
years
number of cases of genital
herpes increased
by 168%.
Etiology
*EtiologyHSV belongs to the family
herpes viruses (Herpesviride).
Genomes of HSV types 1 and 2 by 50%
homologous. Virus type 1
determines mainly
respiratory damage
organs. With the simple virus
herpes type 2 associated
the occurrence of genital
herpes and generalized
infection of newborns.
* The HSV genome is presented
double-stranded DNA. On my
HSV shell has antireceptors,
thanks to which he joins
tissues of ecto- and endodermal
origin (pantropism). HSV,
how a DNA containing virus can
integrate the genetic apparatus
host cells and cause
malignant transformation
cells. Penetration of the virus into
some cells
(for example, in
neurons) not
accompanied by
virus replication
and cell death.
On the contrary, the cell
provides
depressing influence
and the virus goes into
state of latency.
After a while
time may
take place
reactivation that
determines
transition of latent
forms of infection in
manifest. Classification
According to the process:
- primary (symptomatic)
and asymptomatic),
- primary clinical
episode at
existing
genital herpes,
- recurrent
(symptomatic and
asymptomatic).
By localization:
Limited
Generalized
According to clinical
manifestations:
Herpes of skin and mucous membranes
shells
Ophthalmoherpes
Gynecological herpes
Herpetic stomatitis
Herpetic
meningoencephalitis
Generalized (usually
intrauterine) herpes *Source of infection – patient
or a virus carrier.
*Infection with HSV type 2
carried out most often
sexually, less often
contact, transplacental
and transfusion.
*Virus penetration into
entrance gate area
accompanied by damage
epithelium of the skin or mucosa with
subsequent development
regional lymphadenitis and
hematogenous
spreading the virus through
its adsorption on the surface
red blood cells and absorption
leukocytes and macrophages.
Clinic
*Clinic*During primary infection
the incubation period is 1–10 days.
Clinical manifestations last 18–24 days, with
increasing symptoms over the course of a week.
Paresthesia and burning sensation appear in
genital area, neuralgia in the gluteal region,
inguinal femoral areas, dysuria and
last up to 24 hours. Subsequently
viral damage to the epithelium manifests itself as
vesicles on an erythematous background with further
crust formation. Primary herpes is always
occurs with a pronounced general infectious
syndrome: low-grade fever, headache,
sleep disorder, can manifest itself in various ways
lesions of the skin, conjunctiva or cornea
eyes, aphthous stomatitis, acute inflammation
upper respiratory tract.
* In pregnant women, asymptomatic and
atypical forms. Non-primary genital infection occurs
less pronounced, because develops against the background
circulating antiviral antibodies:
shorter duration of clinical manifestations
(up to 15 days), less pronounced
general intoxication syndrome, less often
asymptomatic discharge is observed
virus.
Changes in the placenta
*Changes inplacenta
*Herpetic lesion of the placenta
leads to a whole series
pathomorphological changes. Due to significant structural disturbances
and placental function decreases
supply of oxygen to the fetus,
energy and plastic
materials, which leads to the development
chronic intrauterine hypoxia
and intrauterine growth retardation
fetus
Changes in the placenta
*Changes inplacenta
*Inflammation of the inner lining of blood vessels
stem and intermediate villi with
subsequent obliteration of the lumen;
*Giant cell metamorphosis
syncytiotrophoblast, with the presence
intranuclear inclusions;
*Sclerotherapy of damaged areas
villous chorion;
*Severe developmental delay
placenta;
*Focuses of necrosis in the villous chorion
placenta;
*Hemorrhage in the intervillous
space; Fetal infection during
pregnancy time
happens in two
ways:
- transplacental;
-intranatal (with
going through labor
paths). * Clinical manifestations in the fetus depend on the period
infection and pathogen dose. At primary
genital herpes infects 30–80% of fetuses, and
with recurrent 3–7% of fetuses. Frequency
miscarriage with primary HSV in the first trimester
is 54%, and in the second trimester - 30%, in the third trimester -
10–15%. Intrauterine infection of the fetus in 50%
cases is accompanied by the birth of premature babies
children. In 40% of cases in surviving newborns
organic and dysfunctional
disorders (cerebral palsy, epilepsy, delayed neuropsychic development, developing
immunodeficiency conditions, heart defects,
blindness, deafness, retinal pathology). Intrauterine
herpetic infection:
*Generalized infection involving
into the pathological process of several organs at once
(liver, lungs, adrenal glands): detection frequency –
25%, mortality without treatment - 90%, when
antiviral therapy – 57%, disability among
survivors - up to 85% (visual impairment,
neurological disorders, delay in
mental and physical development, epilepsy,
cerebral palsy, deafness, etc.).
*In the form of local damage to the central nervous system.
Local with damage to the central nervous system (herpetic
meningoencephalitis): detection rate – 35%,
mortality without treatment 56%, when carried out
antiviral therapy – 15%, disability among
surviving children – up to 50%;
*In the form of a mucocutaneous form. Local
with damage to the skin and mucous membranes: frequency of detection
– 45%, mortality without treatment – 18%;
Diagnostics
*DiagnosticsMolecular genetic methods
PCR (polymerase chain
reaction)
LCR (ligase chain reaction)
DOT hybridization method
The advantages are:
high sensitivity (95–
97%), specificity (90–100%).
Material: blood, scraping
epithelial cells from
urethra or cervical
canal, amniotic fluid.
Diagnostics
*Diagnostics*Linked immunosorbent assay
(ELISA).
The ELISA method is based on detection in
venous blood of patients
immunoglobulins class M and G. When
“fresh infection” at the beginning
JgM appear, reaching a maximum at 2
months, then there is a decrease by
background of the appearance and increase of JgG. JgM like
rule are not further defined. JgG
remain with a person for life. At
recurrence of infection may occur
JgM against the background of an increase in JgG titer.
Diagnostics
*Diagnostics* Mutual investment fund (direct method
immunofluorescence) When
immunofluorescent
microscopy revealed
presence of cytoplasmic
inclusions and their
morphological
features, as well as the percentage
infected cells in
smears and scrapings. Mutual Fund has
number of advantages: economically
accessible, specific (90%),
can be completed quickly (1–2
hours). Flaws:
subjective, not always
high quality test systems
Diagnostics
*Diagnostics*Cytological method
Scraping the affected area of skin
stained according to Romanovsky-Giemsa and
detect cells with several
nuclei and inclusions.
Diagnostics
*Diagnostics*Cultural method
* HSV are used for cultivation
chicken embryos. From blisters on the skin
the patient's contents are taken away and
they infect a chicken embryo. For
studying the results take
the corresponding area of the egg and
placed in sterile water. Character
lesions are analyzed by looking at
culture on a dark background.
* Disadvantages: long
and expensive
method
Diagnostics
*DiagnosticsModern diagnostic methods:
1. Pokit
2. Herpeselect
3. Western Blot.
* Pokit - express analysis that detects simplex virus
herpes type 2. Specificity is 94-97%. On
analysis, blood is taken from a finger, analysis results
received within ten minutes.
* Herpeselect includes two methods: ELIZA and
immunoblotting. They are used to detect antibodies to
herpes simplex virus of both types. These tests
can be used during pregnancy. Result
received within one to two weeks after collection
blood from a vein.
* Western Blot detects both types of simplex virus
herpes. It is highly sensitive and
specificity (more than 99%). The result is ready in two
weeks after taking the analysis.
Diagnostics
*Diagnostics*For condition assessment
fetoplacental system
greatest practical
meaning now
echography acquires and
Doppler
velocity curve study
blood flow due to their high
informative, non-invasive,
security and opportunity
use throughout
pregnancy, including
early stages of gestation. Target
research - conduct analysis
hemodynamic disorders in
system "mother-placenta-fetus"
pregnant women who have had a herpes virus infection.
Sonographic signs of IUI
*Echographicsigns of IUI
* Much - or oligohydramnios, hyperechoic suspension
in amniotic fluid, amniotic cords,
villous hypoplasia, thinning of the chorion,
decrease in its echogenicity, placentitis - edema
(thickening), heterogeneous echogenicity
placental parenchyma, blurred boundaries
lobules, signs of premature aging
placenta, nonimmune hydrops fetalis
(subcutaneous edema, pleural and/or
pericardial effusion or ascites,
hydrothorax, parenchymal (hepatic,
splenic) calcifications, defects
development of internal organs, hepato- and
splenomegaly.
Diagnostics
*Diagnostics*Biopsy of trophoblast (chorion) in I
trimester of pregnancy followed by
karyotype study;
*Transabdominal amniocentesis with
subsequent virological
study of amniotic fluid;
*Cordocentesis followed
fetal blood testing for HSV -
infection by at least 2 methods (in
terms 22 – 23 weeks).
To detect HSV in amniotic fluid
use methods to isolate the virus in
culture or PCR.
Treatment
*TreatmentBasic principles of treatment
genital herpes are:
1. Suppression of virus replication with
for the purpose of limiting
spread of infection.
2. Normalization of the immune response
with a view to forming
full protection.
Treatment
*TreatmentThere are currently 2 treatment options
genital herpes: episodic and suppressive.
Episodic therapy
implies oral
taking the drug in the acute phase
process, which reduces
duration of relapse and
is the most effective
form during prodrome or in
at the very beginning of the rash. Such
the regimen is effective in patients with
rare episodic
rashes (once every 6 months). TO
this method can be attributed
stop dose method. This
single dose of the drug
maximum dosage at
first prodromal
symptoms.
Preventive (suppressive)
therapy recommended
patients with frequent
relapses (more than 1 time in 6
months), severe pain
syndrome, when planning
pregnancy. On the background
suppressive therapy, according to
compared to episodic
patients report improvement
quality of life, decrease
relapse rates.
Treatment
*Treatment*During pregnancy with the drug
choice for treatment of HSV is
Acyclovir. This drug is not
has a teratogenic effect on
the fruit is safe and can
can be prescribed from any trimester
pregnancy.
Treatment
*TreatmentImmunomodulatory therapy:
* Interferonogenesis inducers and drugs
interferon (panavir, viferon, cycloferon,
allokin-alpha, longidase.
* Specific immunoglobulins
(normal human immunoglobulin,
sandoglobulin, intraglobin).
* Immunostimulating drugs (thymalin,
taktivin) - activate the T-lymphocyte system,
stimulates the production of lymphokines, in
in particular a- and y-interferons.
* The use of immunomodulators is not indicated
earlier than the 14th day for acute and 7th day for
recurrent process.
Treatment
*TreatmentMetabolic therapy
Considering the presence of metabolic
dysregulation in cells and tissues
mother-placenta-fetus system
viral infection are prescribed
drugs that normalize processes
bioenergy at the cellular level and
stimulating biosynthetic
processes (riboflavin mononucleotide,
lipoic acid, calcium pantothenate,
tocopherol acetate, riboxin, orotate
potassium, pyridoxal phosphate, phytin,
troxevasin).
Treatment
*Treatment* For the treatment of herpetic
infections in the second and third trimesters
pregnancy can be used
plasmapheresis.
* Indications: presence of antigens to HSV in
cervical canal, increased
coagulant properties, violation
rheological blood parameters,
immunological imbalance
parameters, high level in
circulating blood serum
immune complexes and
immunoglobulins M, G, E, A,
clinical and laboratory signs
intrauterine infection and
autoimmune disorders.
*Plasmapheresis can be performed in
any stage of pregnancy. Well
therapy – 2-3 sessions with an interval of 1-3
day.
Preconception preparation
*PregravidPreparation
The basic principles of pregravid
preparations are:
1. Careful collection of anamnesis with the aim
detecting episodes of genital herpes in
women and sexual partner.
2. Examination of both partners using methods
PCR, ELISA, PIF.
3. Prescribing suppressive therapy to a woman
3 months before the planned pregnancy (if
there was a history of relapses of herpes).
4. To a partner with a history of episodes
herpes, suppressive therapy is prescribed for
throughout pregnancy.
Pregnancy is planned only when
persistent and long-term (more than 6 months) remission
herpetic infection
Vaccine
*Vaccine* The vaccine "Vitagerpavak" (Moscow) is
inactivated antigen of herpes simplex virus types 1 and 2.
* Vaccination of chronically infected people with HSV
is accompanied by a 3-4-fold increase in the specific Tkiller activity of lymphocytes, promotes stimulation
high activity of NK cells and cessation of viremia.
* The effectiveness of the vaccine has been confirmed by clinical and laboratory tests
trials: relapses of the disease completely stopped in
63% of patients began to occur quite less frequently in 27% and not
the relapse rate of 8% of patients changed.
*
The vaccine is used in the remission stage, no earlier than after 5
days after complete disappearance of clinical manifestations
herpetic infection. Injected intradermally into the area
the inner surface of the forearm in a single dose of 0.2 ml.
Vaccination course for herpetic infections of the skin and mucous membranes
consists of 5 injections, which are carried out at intervals of 7 days.
Patients with complicated herpetic infection (relapses - 1 and
more than once a month) 2nd and subsequent injections are repeated with
at intervals of 10 days. After 6 months a repeat course is carried out
vaccinations (5 injections). 1. During primary infection during
pregnancy:
- in the first trimester (risk of intrauterine infection
90–95%) – the issue of termination of pregnancy is being resolved;
- 6 weeks before birth (75% risk) – delivery
- in 1–2 weeks. before birth (risk 1-3%) – delivery
by cesarean section.
2. If genital herpes recurs during
pregnancy (risk 0.1%):
- regardless of the trimester, episodic
Acyclovir therapy according to the standard regimen.
When identifying herpetic rashes during
childbirth in the genital area - delivery by
Caesarean section operations; if there are no rashes - childbirth
through the natural birth canal.
 Order 343 mail. Order by Russian post. Consequences of failure to appear in court when summoned
Order 343 mail. Order by Russian post. Consequences of failure to appear in court when summoned How to put a password on a folder on a Windows computer without and with programs
How to put a password on a folder on a Windows computer without and with programs Pluton – Free Bootstrap HTML5 One Page Template
Pluton – Free Bootstrap HTML5 One Page Template History of ZX Spectrum: Myths and reality New Spectrum
History of ZX Spectrum: Myths and reality New Spectrum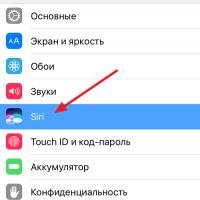 Voice assistant Siri from Apple Siri functions on iPhone 6s
Voice assistant Siri from Apple Siri functions on iPhone 6s How to roll back to a previous version of iOS?
How to roll back to a previous version of iOS? Unlock iPad in four days
Unlock iPad in four days